My COVID-19 reading
5/27/2020
- Infection Control
- Fitted N-95 respiratory along with other PPEs and negative pressure room for aerosol-generating procedures
Aerosol-generating procedures in the ICU include: endotracheal intubation, bronchoscopy, open suctioning, administration of nebulized treatment, manual ventilation before intubation, physical proning of the patient, disconnecting the patient from the ventilator, non-invasive positive pressure ventilation, tracheostomy, and cardiopulmonary resuscitation.
- Surgical/medical masks along with other PPEs for non-aerosol-generating procedures.
- Video-guided laryngoscopy for endotracheal intubation by experienced provider.
- Fitted N-95 respiratory along with other PPEs and negative pressure room for aerosol-generating procedures
- Resuscitation in patients with COVID-19 and shock
- There are very low-quality evidence regarding restricted vs. liberal use of fluid resuscitation. Clinician should constantly assess fluid responsiveness and status of ARDS when administering fluid resuscitation.
- Norepinephrine should be used as the first-line vasoactive agent. If not available, vasopressin or epinephrine can be used.
- Vasopressin is the recommended second-line agent.
- MAP goal for vasoactive agents should be 60-65mmHg.
- When cardiac dysfunction is present and hypoperfusion not responding to norepinephrine alone, dobutamine is suggested over increasing norepinephrine dose.
- Corticosteroid for shock is recommended, typical dosing hydrocortisone 200mg qd.
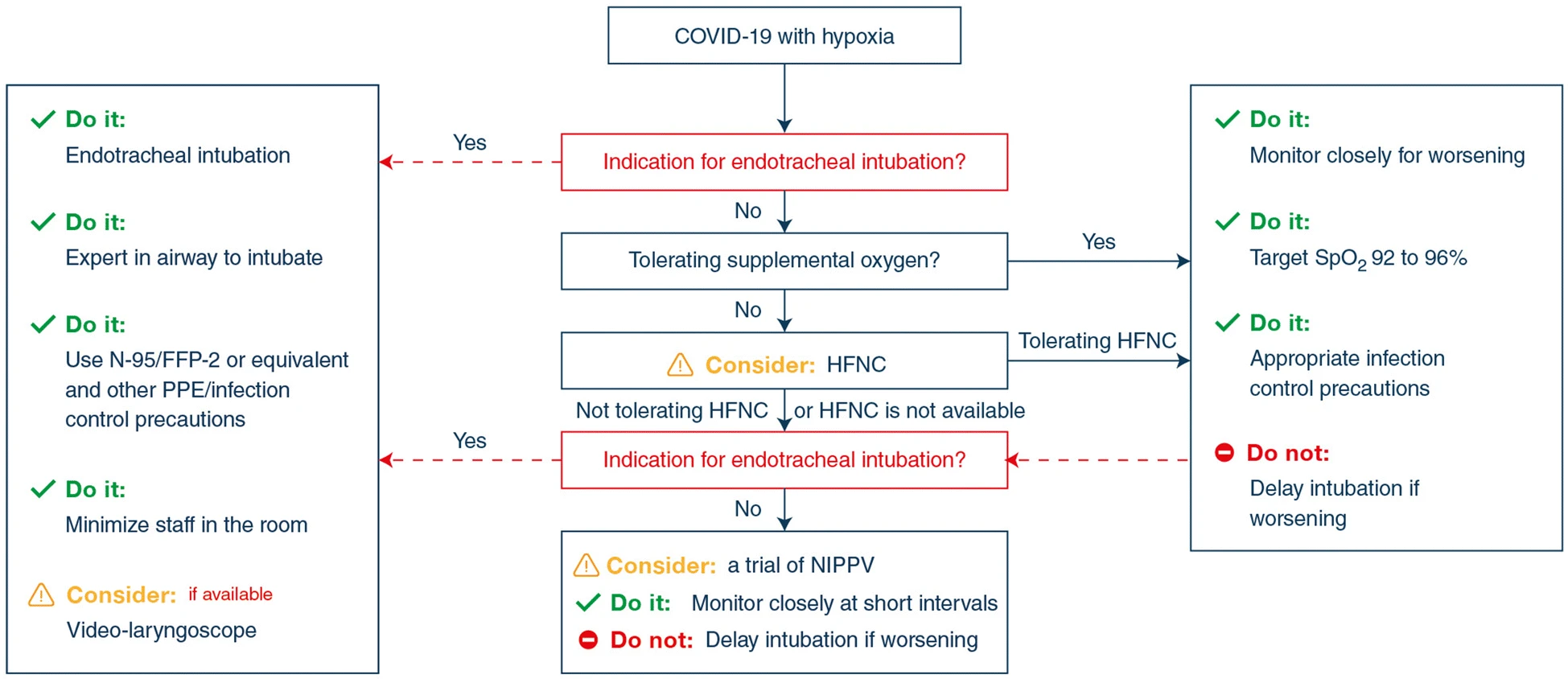
- Managing respiratory failure
- Supplemental O2 is recommended when SpO2 is below 92%. Goal of SpO2 should be no higher than 96%.
- HFNC not NIPPV should be attempted if failed conventional nasal oxygen
- For vented patients with ARDS, low tidal volume ventilation is recommended.
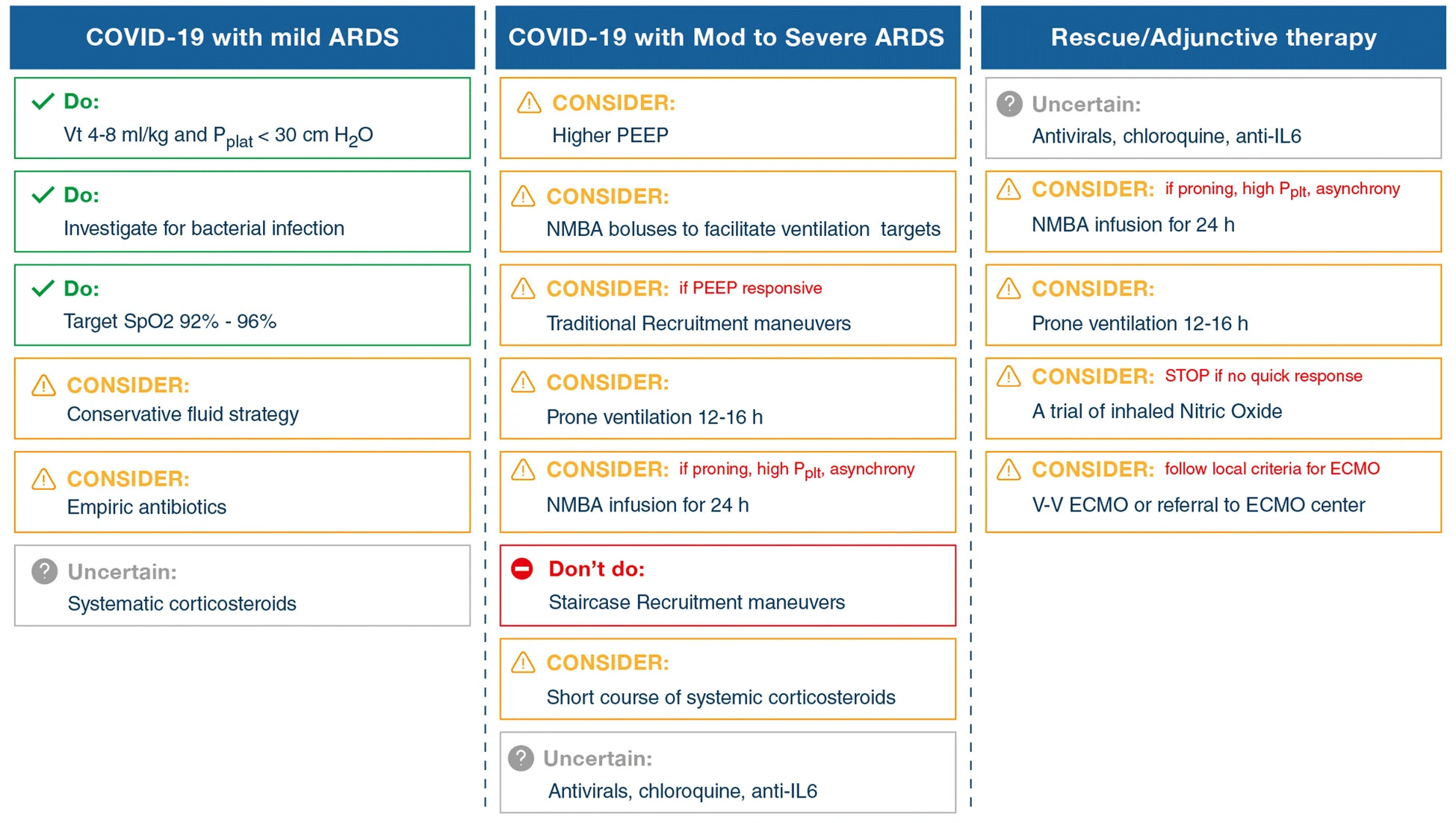
- Target plateu pressure should be < 30mmH2O.
- Higher PEEP strategy is recommended.
- Prone ventilation is recommended in those with moderate to severe ARDS for 12-16 hours
- As needed intermittent boluses of neuromuscular blocking agents can be used for moderate to severe ARDS
- In the event of persistent ventilator dyssynchrony, the need for ongoing deep sedation, prone ventilation, or persistently high plateau pressures, we suggest using a continuous NMBA infusion for up to 48 hours
- Pulmonary vasodilator may be used as a rescue therapy
- Inhaled nitric oxide has potential harm and no clear mortality benefit, therefore it is not recommended. It could cause rebound pulmonary vasoconstriction.
- Traditional recruitment maneuvers can be used for persistent hypoxia.
- VV-ECMO if nothing works
- COVID-19 treatment
- Cytokine Storm Syndrome: In vented patients, the presence of ARDS could justify systemic corticosteroids use.
- Empiric antibiotics should be given for patients with COVID-19 and respiratory failure
- Routine use of IVIG is not recommended
- Routine use of convalescent plasma is not recommended. Efficacy and safety is unclear.
- Routine use of lopinavir/ritonavir is not recommended. In a recent trial from China, the drug did not significantly reduce 28-day mortality. The drug has generally good safety profile, but may have interactions with many drugs
- In ICU patients, there is insufficient evidence to issue a recommendation regarding antiviral agents for COVID-19. More evidence is needed for remdisivir, rIFNs, and chloroquine or hydroxychloroquine, and tocilizumab.